Irritable Bowel Syndrome (IBS) is a common digestive disorder that affects over 35 million Americans, causing symptoms like bloating, gas, abdominal pain, diarrhea, and constipation. While most people associate antibiotics with treating infections, you may be surprised to learn that some doctors prescribe antibiotics for IBS—especially IBS-D (diarrhea-predominant IBS).
So, why would your doctor give you antibiotics if IBS isn’t caused by a bacterial infection? In this article, we’ll explore the science behind this treatment approach, when it’s appropriate, and whether it’s truly effective.

Understanding the Link Between IBS and Gut Bacteria
One of the most important discoveries in recent years is the role of the gut microbiome—the trillions of bacteria that live in your digestive tract. In people with IBS, especially IBS-D, these bacteria may become imbalanced, leading to a condition known as Small Intestinal Bacterial Overgrowth (SIBO).
SIBO occurs when bacteria that are normally found in the colon migrate into the small intestine, where they ferment food too early in the digestive process. This results in gas production, bloating, and diarrhea—classic IBS symptoms.
In these cases, doctors may prescribe antibiotics to reduce the overgrowth of bacteria and relieve symptoms.

What Antibiotic Is Most Commonly Used for IBS?
The most commonly prescribed antibiotic for IBS is Rifaximin (brand name: Xifaxan). It’s a non-systemic antibiotic, meaning it stays in the gut and isn’t absorbed into the bloodstream—making it a safer choice for long-term gut health.
Key facts about Rifaximin for IBS:
- Often used when SIBO is suspected
- Approved by the FDA for IBS-D
- Typically taken for 10–14 days
- May reduce symptoms like bloating, gas, and loose stools
Does Rifaximin Work for IBS?
Clinical trials have shown that Rifaximin can significantly reduce IBS-D symptoms, particularly bloating and diarrhea. However, the benefits may be temporary, and many patients find that symptoms return after a few months.
In some cases, patients require repeated courses of Rifaximin, which can raise concerns about long-term antibiotic use and bacterial resistance.
Risks of Using Antibiotics for IBS
While antibiotics can offer short-term relief, they come with potential downsides:
Antibiotic Resistance:
Repeated use of antibiotics increases the risk of resistant bacteria, making future infections harder to treat.
Disruption of Gut Microbiome:
Antibiotics kill both harmful and beneficial bacteria, which may lead to microbiome imbalance or worsen gut health in the long run.
Recurrent Symptoms:
Many IBS patients report symptom relapse after finishing antibiotics, especially without addressing the root cause.
Are There Alternatives to Antibiotics for IBS?
Yes. More and more doctors and functional medicine practitioners are turning to gut-focused probiotics, dietary changes, and targeted antimicrobial herbs to support the gut microbiome without the side effects of antibiotics.
One emerging option is the use of spore-based probiotics, which are particularly resilient and effective in balancing the gut.
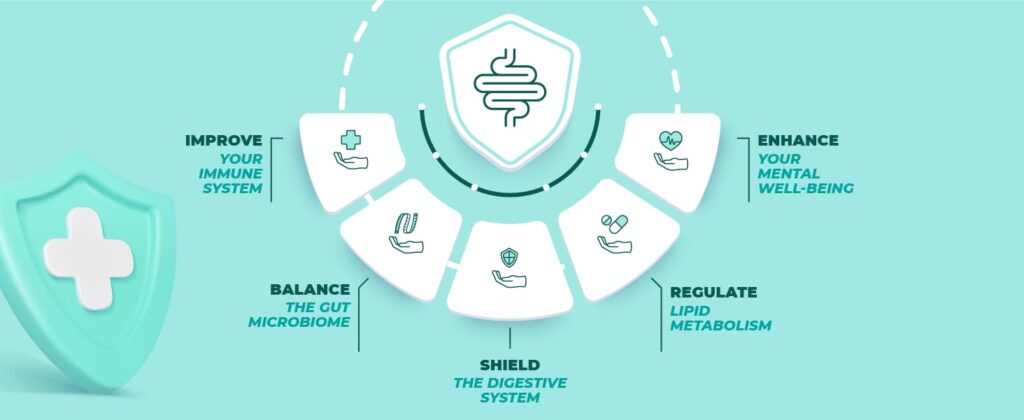
A New Approach: GutShield – Liquid Spore Probiotic

If you’re looking for a more sustainable and natural way to support your gut health, consider GutShield – Liquid Spore Probiotic.
🟢 Why GutShield?
- Contains clinically studied Bacillus spores that survive stomach acid
- Helps restore microbial balance after antibiotic use
- Supports healthy digestion and reduces bloating
- No refrigeration needed & easy to use
Whether you’ve taken antibiotics for IBS or are seeking a natural alternative, GutShield is designed to support your digestive health from the inside out.
When Should You Talk to Your Doctor About Antibiotics for IBS?
You may want to ask your doctor about antibiotics like Rifaximin if:
- You’ve been diagnosed with IBS-D
- You suspect SIBO based on symptoms
- Other IBS treatments haven’t worked
- You’re experiencing severe bloating and diarrhea
It’s important to combine antibiotics with a comprehensive treatment plan that may include diet changes, probiotics, and lifestyle adjustments for long-lasting relief.
Takeaway
While antibiotics like Rifaximin can help relieve IBS-D symptoms, they are not a cure and often provide temporary relief. They may be appropriate for treating bacterial overgrowth, but should be used with caution.
For a more holistic and long-term approach to managing IBS, consider spore-based probiotics like GutShield, which help rebalance your gut microbiome without the risks associated with antibiotics.






